Staging a Rescue
Anterior capsular tears can complicate cataract surgery at any stage. These tears fall into two categories: primary tears occur during capsulorhexis creation, while secondary tears develop after completion. Surgeons often encounter primary tears in cases of intumescent white cataracts, pseudoexfoliation, and pediatric cataracts.
If a tear occurs during a continuous curvilinear capsulorhexis and remains visible at the capsule’s edge without extending beyond the pupil margin, surgeons can use rescue maneuvers. These include regrasping the flap and redirecting forces to counteract the tear. If the tear extends beyond the pupil margin, careful evaluation determines whether it stays pre-equatorial or compromises the posterior capsule.
Case Example
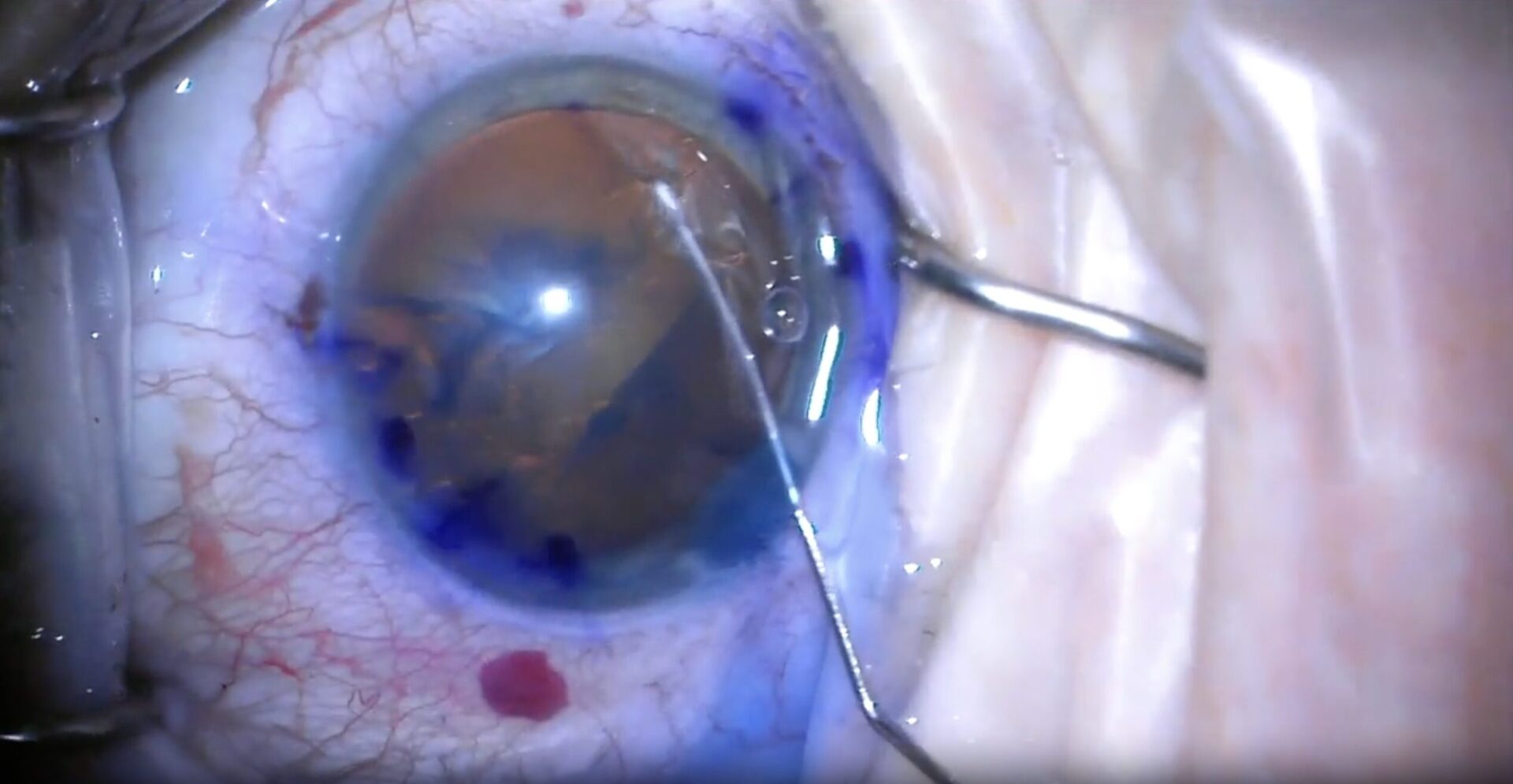
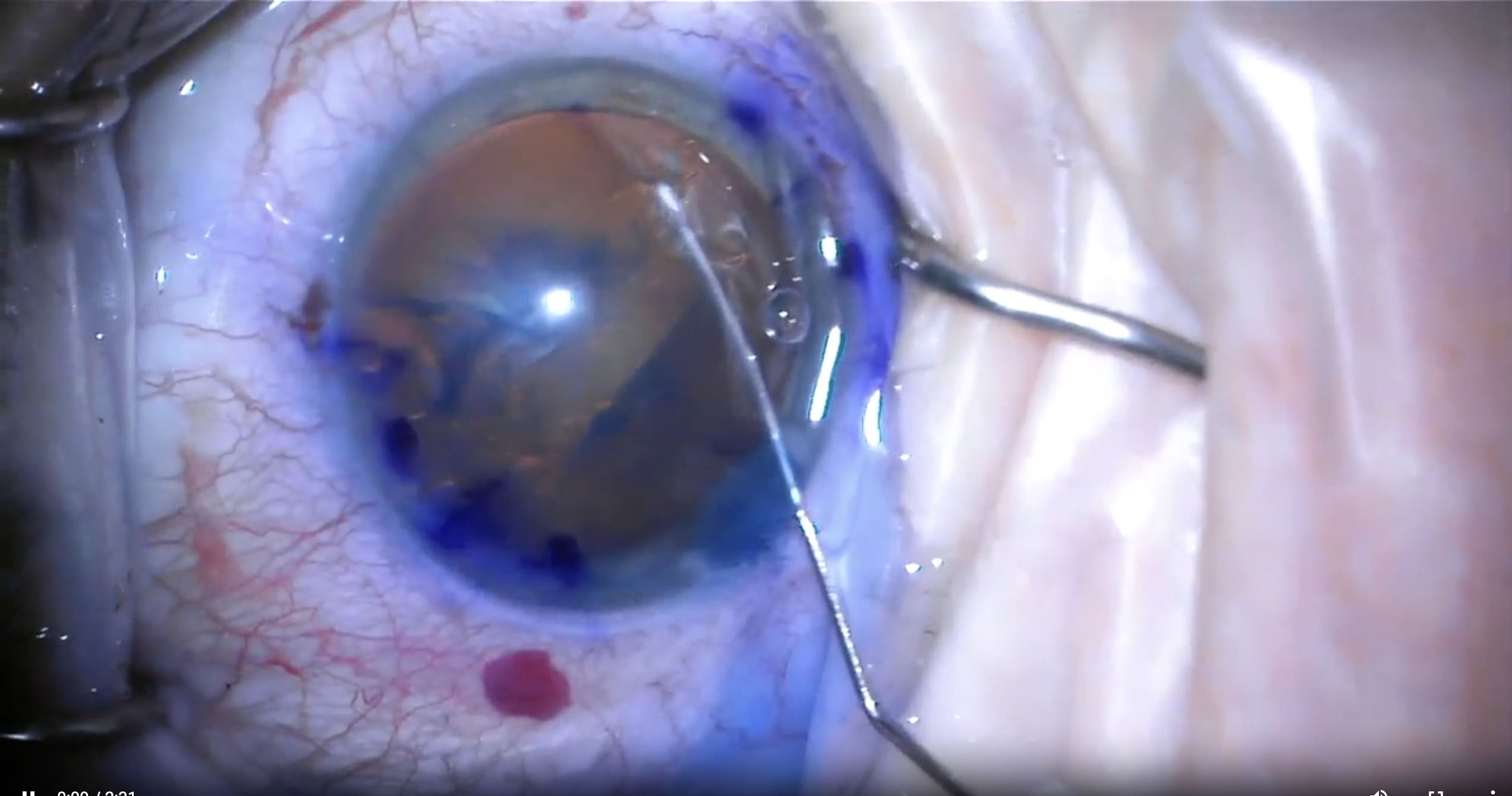
In the video example, a large anterior capsular tear developed early in capsulorhexis creation. It extended beyond the pupil margin, posing a high risk of posterior capsule compromise, though no immediate signs indicated such involvement.
Staging a Rescue
Completing the Capsulorhexis
To enable lens removal, I first completed the capsulorhexis. This step was challenging because the tear reduced the tension needed for the curvilinear technique. In such cases, the can-opener or multipuncture approach may be necessary. These methods use a cystotome or bent needle to create small incisions on both sides of the tear, forming an opening in the anterior capsule.
Preventing Posterior Extension
The next challenge was preventing posterior tear extension during phacoemulsification. To reduce this risk, I avoided hydrodissection and performed nucleus debulking through hydrodelineation. As shown in the video, I injected OVD into the capsular bag behind the lens, causing slight prolapse into the anterior chamber. Using a bimanual technique, I debulked the lens with both a chopper and an OVD cannula.
IOL Placement and Final Steps
I inserted a three-piece IOL into the sulcus, leaving the trailing haptic outside the main corneal incision as a precaution. This allowed for easy retrieval if the tear extended posteriorly and compromised capsular support. This approach, known as the scaffold technique, stabilizes the anterior chamber, protects the posterior capsule, and enables deeper plane phacoemulsification.
After completing phacoemulsification at the iris plane and confirming capsule integrity, I repositioned the IOL inside the capsular bag. Residual cortical material was easily removed using irrigation and aspiration around and under the IOL.
Despite the unplanned complication, the patient had an excellent outcome.
Signs of Posterior Capsule Extension
Signs that a tear has reached the posterior capsule include:
- Deepening of the anterior chamber
- The pupil snap sign
- Sudden peripheral red reflex appearance
- Loss of flap motility
- Nucleus tilt or nucleus sink
If the anterior capsular tear remains pre-equatorial, phacoemulsification can still proceed based on the surgeon’s experience. If necessary, conversion to extracapsular cataract extraction or small-incision cataract surgery remains an option.