Laser Offers a Reliable Alternative to Eye Drops to Treat Glaucoma or Ocular Hypertension: The Results of the LiGHT Study
Glaucoma is a chronic eye condition requiring lifelong monitoring and management. Many patients control intraocular pressure (IOP) with medication, particularly eye drops. However, this approach has challenges. Complications, side effects, and adherence issues reduce effectiveness. Some patients do not respond to medications, experience reduced effectiveness over time, or find the cost too high.
Why Consider SLT?
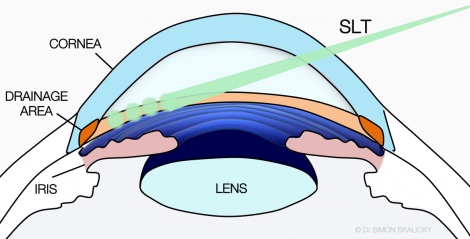
Adherence to medication is a major concern. Studies show that 20% to 66% of glaucoma patients do not use their medication as directed. Laser therapy for glaucoma, such as selective laser trabeculoplasty (SLT), offers a perfect compliance alternative. SLT uses low-energy nanosecond pulses in a controlled manner. It targets the trabecular meshwork (TM) to improve aqueous outflow and lower IOP.
Compared to other laser treatments, SLT has larger spot sizes and lower power density. This results in minimal thermal damage to surrounding tissues. Standard argon laser trabeculoplasty (ALT) uses much higher energy. SLT, in contrast, applies only about 1 mJ per pulse. This precise energy application confines heat to a small area. It reduces collateral damage risk and allows for repeated treatments if needed.
The Importance of the LiGHT Study
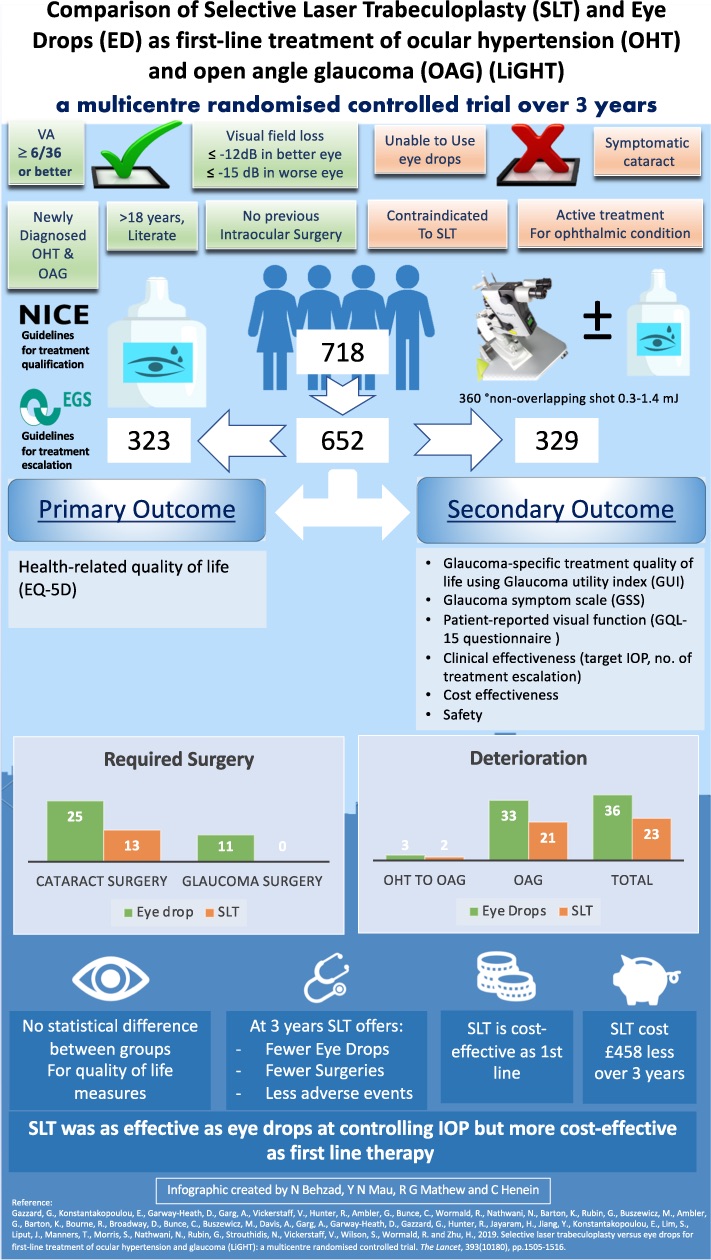
The LiGHT (Laser in Glaucoma and Ocular Hypertension) study reshaped glaucoma treatment. This multicenter, randomized controlled trial assessed quality of life, IOP control, disease management, and the need for surgery.
Three-Year Results
The study ran from 2012 to 2014 and included 718 patients with mild to moderate glaucoma. Half received SLT first, while the other half started with medication. The primary outcome was health-related quality of life. Other measures included IOP control and the need for surgery. Notably, 78% of eyes treated with primary SLT remained drop- and surgery-free after three years. Most patients needed only one SLT treatment. The IOP control effect diminished over time. However, repeat treatments were equally effective. This suggests SLT is a viable long-term glaucoma management strategy.
Six-Year Extension
An extension of the study included 88% of the original participants. Those initially treated with SLT could receive up to three treatments. Patients on medication could switch to SLT. The results were compelling. Seventy percent of the SLT-first group maintained target IOP without medications. Disease progression was slower. Time to surgical intervention was longer compared to the medication-first group.
Conclusion
SLT has demonstrated its ability to control IOP effectively and safely in patients with mild to moderate open-angle glaucoma. The LiGHT study’s findings support SLT as a primary intervention, potentially reducing the need for ongoing medication and delaying or preventing the need for surgery. While questions about the optimal frequency of SLT treatments and post-laser drug regimens remain, laser therapy for glaucoma should be a strong consideration for newly diagnosed patients or those in the early stages of the disease. By integrating SLT into glaucoma management, patients can benefit from a more straightforward, compliance-friendly treatment that offers sustained IOP control and improves long-term outcomes.