Eye Pain That’s More Than Dry Eye: Understanding Neuropathic Ocular Pain
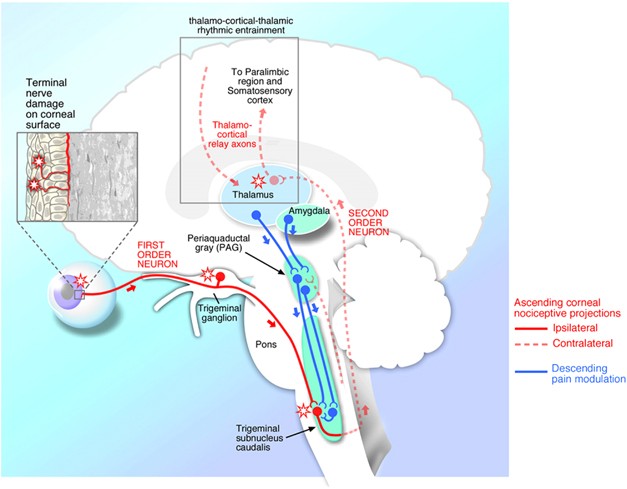
Ever experienced a persistent burning or stinging sensation in your eyes that just won’t go away? It might be more than just dry eyes or a common eye infection. You could be dealing with neuropathic ocular pain (NOP). This condition arises from nerve dysfunction in the eye’s surface or the pathways connecting the eye to the brain, causing chronic and often debilitating pain.
 What Causes Neuropathic Ocular Pain?
What Causes Neuropathic Ocular Pain?
NOP can develop due to several factors:
- Ocular Surgeries: Procedures like refractive surgery or cataract extraction can sometimes trigger NOP.
- Infections: Post-herpetic neuralgia, for instance, is a complication of herpes zoster affecting the eye.
- Chronic Ocular Conditions: Long-term issues like inflammation or tear deficiency can lead to nerve problems.
- Idiopathic Causes: Sometimes, NOP occurs without a clear reason.
- Associated Conditions: Other pain conditions, such as migraines or fibromyalgia, or trauma like a traumatic brain injury, can also contribute to NOP.
How Does It Feel?
People with NOP often describe their pain as burning, stinging, or aching. They might also experience heightened sensitivity to light (photophobia) or wind, making everyday activities uncomfortable. Unlike typical eye conditions, the symptoms of NOP usually outweigh the visible signs, making diagnosis tricky.
Diagnosing NOP
Identifying NOP involves a thorough examination of the eye surface and tear quality to rule out other causes of pain, like tear deficiency or inflammation. Special questionnaires, like the Neuropathic Pain Symptom Inventory (NPSI)-Eye, can help pinpoint neuropathic pain characteristics. If NOP is suspected, an “anesthetic challenge test” can help determine if the pain is peripheral (related to the eye surface) or central (related to the brain pathways).
Treatment Options
The treatment for NOP depends on whether the pain is peripheral or central. Here’s a breakdown:
- Peripheral NOP: For pain originating from the eye surface, treatments like autologous serum tears, which use a patient’s blood components, can help regenerate nerves.
- Central NOP: When the pain is linked to brain pathways, oral medications such as pregabalin, gabapentin, or duloxetine may be prescribed. These neuromodulators can help manage pain but require patience, as they might take a few months to show results.
- Adjuvant Therapies: For associated symptoms like light sensitivity or headaches, treatments used for migraines, such as transcutaneous electrical nerve stimulation or botulinum toxin injections, can be beneficial. In cases of cutaneous allodynia (pain from light touch around the eye) or post-surgical pain, periocular nerve blocks with a combination of corticosteroids and long-acting anesthetics can provide relief.
Holistic Approach
Because NOP can also lead to anxiety, depression, and other mood disorders, managing this condition often requires a holistic approach. Complementary therapies such as acupuncture, cognitive behavioral therapy, or even hypnosis can be valuable additions to the treatment plan.
The Road to Relief
Dealing with NOP can be challenging, but understanding the condition and its treatment options is a crucial first step. If you or someone you know is experiencing these symptoms, don’t hesitate to seek help from a specialist. A multidisciplinary approach, involving ophthalmologists, pain specialists, neurologists, and mental health professionals, is often the best way to manage this complex condition.
Remember, while the road to relief may be long, with the right combination of treatments and support, it’s possible to regain control and improve your quality of life.
Please schedule an appointment with our ophthalmology team





 What Causes Neuropathic Ocular Pain?
What Causes Neuropathic Ocular Pain?
