OCT and Early Alzheimer’s Diagnosis
Alzheimer’s disease is a progressive neurodegenerative disorder and a leading cause of dementia worldwide. It is characterized by memory loss, cognitive decline, and behavioral changes. Early detection is crucial because it helps improve patient outcomes and manage disease progression more effectively. Currently, diagnostic methods include neuroimaging and cognitive assessments. However, advancements in ophthalmic technology, such as Optical Coherence Tomography (OCT), are now offering promising new pathways for early and non-invasive diagnosis.
What Is OCT?

Optical Coherence Tomography (OCT) is an advanced imaging technique that captures detailed cross-sectional images of the retina. It allows ophthalmologists to visualize the different layers of the retina with micrometer resolution, enabling the identification of subtle structural changes. In recent years, researchers have identified connections between retinal abnormalities and neurodegenerative conditions, including Alzheimer’s disease.
The Retina-Brain Connection
The retina, an extension of the central nervous system, shares embryological origins and structural similarities with the brain. This connection means changes in the brain due to Alzheimer’s disease may also manifest in the retina. These changes can include thinning of specific retinal layers and abnormalities in the retinal nerve fiber layer (rNFL) and ganglion cell layer (GCL). OCT provides a unique opportunity to monitor these changes, potentially serving as an early biomarker for Alzheimer’s.
Retinal Findings in Alzheimer’s Disease
 Research has shown that patients with Alzheimer’s disease often exhibit:
Research has shown that patients with Alzheimer’s disease often exhibit:
- Thinning of the Retinal Nerve Fiber Layer (rNFL): Studies suggest that the rNFL—composed of the axons of retinal ganglion cells—may show significant thinning in Alzheimer’s patients. This thinning correlates with disease severity and duration.
- Ganglion Cell Layer (GCL) Abnormalities: OCT can detect changes in the ganglion cell complex, which includes the GCL, inner plexiform layer, and other associated layers. These changes are thought to reflect neurodegenerative processes occurring in the brain.
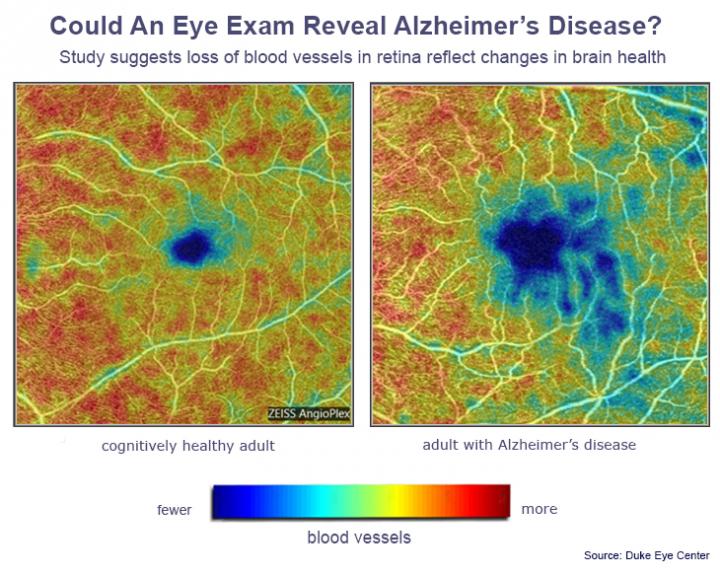
- Reduction in Retinal Blood Flow: OCT angiography (OCTA), an extension of traditional OCT, has highlighted reduced retinal blood flow in Alzheimer’s patients, suggesting microvascular involvement in the disease.
OCT’s Role in Early Diagnosis
OCT provides several advantages for early Alzheimer’s detection:
- Non-Invasive: Unlike traditional neuroimaging methods, OCT is quick, painless, and does not require exposure to radiation or contrast agents.
- Accessibility: OCT devices are widely available in ophthalmology clinics, making this technology accessible to a broader patient population.
- Cost-Effective: Compared to MRI or PET scans, OCT is a more affordable option for monitoring patients at risk of Alzheimer’s.
Future Directions and Limitations
While OCT shows promise, it is not without limitations. Retinal changes may overlap with other neurodegenerative or ophthalmic conditions, potentially complicating the interpretation of results. Additionally, more large-scale studies are needed to standardize diagnostic criteria and validate OCT’s reliability as a screening tool for Alzheimer’s.
Despite these challenges, the integration of OCT into routine eye exams could revolutionize early detection efforts. As ongoing research clarifies its role, OCT may become an essential tool in the fight against Alzheimer’s disease.
What This Means for Patients
Regular comprehensive eye exams are more important than ever. If you or a loved one are experiencing cognitive changes or are at risk for Alzheimer’s, speak with your ophthalmologist about the potential role of OCT in your care. Early detection can make a difference, empowering you to take proactive steps in managing your health.
At PEC, we are committed to leveraging the latest advancements in eye care to benefit our patients. Schedule an appointment today to learn more about how we can help protect your vision and overall health.